Blood Tests
|
This page is especially for those who receive a copy of their blood test results. If you are a New Zealand liver transplant patient and you have more blood tests than immediately below, please email us and we will do our best to cover your results too. Here are the areas covered to date: BIOCHEMISTRY LIVER/ENZYMES RENAL PROTEINS HAEMATOLOGY and, of course, Tacrolimus or Sirolimus |
|
| LIVER FUNCTION TESTS
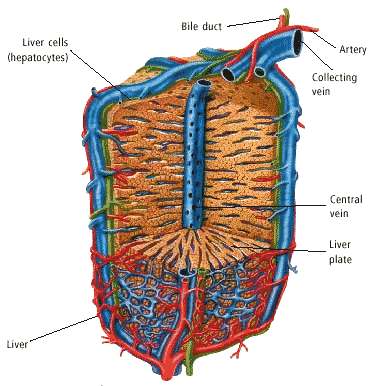
The term "Liver Function Tests" and its abbreviated form "LFTs" is a commonly used term that is applied to a variety of blood tests that assess the general state of the liver and biliary system. Routine blood tests can be divided into those tests that are true LFTs, such as serum bilirubin, serum albumin or prothrombin time, or those tests that are simply markers of liver or biliary tract disease, such as the various liver enzymes (e.g. ALT, AST, alk phos and GGT). In addition to the usual liver tests obtained on routine automated chemistry panels, physicians may order more specific liver tests such as viral serologic tests or autoimmune tests that, if positive, can determine the specific cause of a liver disease. There are two general categories of "liver enzymes." The first group includes the alanine aminotransferase (ALT) and the aspartate aminotransferase (AST). These are enzymes that are indicators of liver cell damage. The other frequently used liver enzymes are the alkaline phosphatase (alk. phos.) and gamma-glutamyltranspeptidase (GGT) that indicate obstruction to the biliary system, either within the liver or in the larger bile channels outside the liver. Return to TOP |
| THE LIVER GROUP OF TESTS
Bilirubin The main bile pigment in humans which, when elevated, causes the yellow discoloration of the skin and eyes called jaundice. Bilirubin is formed primarily from the breakdown of a substance in red blood cells called "heme." It is taken up from blood processed through the liver, and then secreted into the bile by the liver. Normal individuals have only a small amount of bilirubin circulating in blood (less than 12 mg/litre). An increase in the level of bilirubin may be caused by the decreased removal of bilirubin from the blood stream due to liver disease, or the increased destruction of red blood cells. Levels greater than 30 mg/l are usually noticeable as jaundice. The bilirubin may be elevated in many forms of liver or biliary tract disease, and thus it is also relatively nonspecific. However, serum bilirubin is generally considered a true test of liver function, since it reflects the liver's ability to take up, process, and secrete bilirubin into the bile. Alk Phos (alkaline phosphatase) and GGT (gamma-glutamyltranspeptidase) Alk Phos and GGT bloodstream levels are elevated in a number of disorders that affect the drainage of bile, such as a gallstone or tumour blocking the common bile duct, by alcoholic liver disease or drug-induced hepatitis, or by having the flow of bile blocked in smaller bile channels within the liver. The alkaline phosphatase is also found in other organs, such as bone, placenta, and intestine. For this reason, the GGT is utilized as a supplementary test to be sure that the elevation of alkaline phosphatase is indeed coming from the liver or the biliary tract. In contrast to the alkaline phosphatase, the GGT is not elevated in diseases of bone, placenta, or intestine. Mild or moderate elevation of GGT in the presence of a normal alkaline phosphatase is difficult to interpret and is often caused by changes in the liver cell enzymes induced by alcohol or medications, but without causing injury to the liver. ALT and AST (Alanine aminotransferase and aspartate aminotransferase) The ALT and AST are enzymes that are located in liver cells and can make their way into the bloodstream by leaking out of liver cells that are injured. The ALT is thought to be a more specific indicator of liver inflammation, since the AST may be elevated in diseases of other organs such as the heart or muscle. In acute liver injury, such as acute viral hepatitis, the ALT and AST may be elevated to the high 100s or over 1,000 Units/litre. In chronic hepatitis or cirrhosis, the elevation of these enzymes may be minimal (less than 2-3 times normal) or moderate (100-300 U/L). Mild or moderate elevations of ALT or AST are nonspecific and may be caused by a wide range of liver diseases. ALT and AST are often used to monitor the course of chronic hepatitis and the response to treatments such as prednisone and interferon. Return to TOP |
| RENAL TESTS
Creatinine level checks are widely used as a test of renal (kidney) function both as a general screen, along with urine protein, for kidney disease, as a test for serial monitoring of kidney function and where there is potential or actual kidney disease. For patients under renal treatment, creatinine tests monitor established renal disease, renal transplant rejection, renal dialysis and the effects of medications that are potentially harmful to the patient's kidneys. Sodium is the major positive ion of body fluids. The concentration of sodium in body fluids is about thirty times the level inside body cells. The sodium ion content of the blood is a result of a balance between dietary intake and renal excretion. Only a small percentage is lost through the stool or sweat. Many factors affect sodium levels, including the steroid hormone aldosterone, which decreases loss of sodium in the urine. ANP (atrial natriuretic protein) is a hormone secreted from the heart that increases sodium loss from the body. Water and sodium are interrelated - retention of increased sodium is followed by retention of fluid and vice versa. However, the body is able to regulate sodium and water separately if necessary, controlling sodium by means of aldosterone and ANP and water by ADH (antidiuretic hormone). Electrolytes: Potassium Potassium is the major positive ion within cells and it is particularly important for maintaining the electric charge on cell membranes, necessary for neuromuscular communication, for transporting nutrients into cells and for removing waste products from cells. The concentration of potassium inside cells is about 30 times that outside, in body fluids. Aldosterone, a steroid hormone secreted from the adrenal gland, increases levels of potassium excretion. In metabolic acidosis, as caused by uncontrolled diabetes, potassium levels reduce. Alkalosis, as caused by excess vomiting, increases potassium levels. Small changes in the potassium levels outside cells can have substantial effects on the activity of nerves and muscles, particularly with the heart muscle. Low levels cause increased cardiac activity, which can lead to heart arrhythmia, whereas high levels decrease heart activity. In extreme circumstances either situation may lead to cardiac arrest. Taking potassium supplements or potassium-rich drugs is no danger to normal people because their kidneys can efficiently dispose of the excess. Potassium increasers: Kidney failure, very high platelet or white blood cell counts, salt substitutes, some antibiotics, vigorous exercise, pregnancy, some diuretics, lithium. Return to TOP |
| PROTEINS
Blood contains large amounts of proteins, substances made up of small components called amino acids. This test measures the total amount of blood protein and the amounts of the two main protein groups, albumin and globulin which indicate the general state of nutrition and can provide clues to help diagnose some diseases. Albumin is produced mainly in the liver. It helps transport some drugs and other substances through the blood and can be broken down to assist with tissue growth and healing. It also helps prevent blood from leaking out of blood vessels, so when albumin levels drop, oedema may develop, with fluid collecting in the ankles, lungs, or abdomen. Globulin is made up of different proteins formed by the liver and by the immune system. They have many functions, including transporting metals such as iron in the blood, binding themselves to free haemoglobin and providing a defence against infection. Your albumin to globulin ratio is calculated by dividing the amount of albumin by the amount of globulin. Normally, blood contains more albumin so the resulting ratio is normally a value greater than one. Return to TOP |
| HAEMOTOLOGY
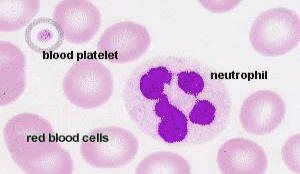
Haemoglobin The oxygen-binding protein within red blood cells. It contributes about 30% of the cell's weight. The lifespan of a red blood cell is 100-120 days. PCV = Packed Cell Volume. MCV = Mean* Corpuscular Volume (*Mean = average) MCH = Mean Corpuscular Haemoglobin WBC = White Blood Cell Count (White blood cells form the family of Leukocytes, which are of two types, granular and non-granular, based on the appearance of their cell contents under magnification. All granular cells have mobility). Neut seg (Segment Neutrophil) [granular type] 50%-70% of White Blood Cells (WBC) Neutrophils play a central role in inflammatory processes. Large numbers invade sites of infection and begin to envelop and destroy tissue debris and foreign bodies, e.g. bacteria. They are the first wave of cells invading sites of infection, and their activity is stimulated if invading micro-organisms are "tagged" with antibodies. Neutrophils cannot replenish their store of granules. The cells die once their supply of granules has been exhausted. Dead neutrophils and tissue debris are the major components of pus. Their lifespan is only about one week. Lost neutrophils are quickly replenished from a reserve population in the bone marrow. Lymphocyte [non-granular type] 20%-40% of WBC Most lymphocytes in the blood stream belong to either the group of B-lymphocytes (~5%) or the group of T-lymphocytes (~90%). Upon exposure to antigens by antigen-presenting cells and T-helper cells (a special group of T-lymphocytes) the B-lymphocytes differentiate into antibody producing plasma cells. The amount of cytoplasm increases and RER fills a large portion of it. T-lymphocytes represent the "cellular arm" of the immune response (cytotoxic T cells) and may attack foreign cells, cancer cells or cells infected by a virus. Another much less frequent medium-sized or large lymphocyte may re-present as natural killer cells which belong to the group of large granular lymphocytes, or as haemopoietic stem cells of which a few will be circulating in the blood stream. Basophil [granular type] 0%-2% of WBC Heparin and histamine dilate the blood vessels, make vessel walls more permeable and prevent blood coagulation. As a consequence, they facilitate the access of other leucocytes and of plasma-borne substances of importance for the immune response to the tissue - e.g. access of neutrophils and antibodies to a site of infection. The release of the contents of the granules of basophils is receptor-mediated. Basophils do not produce antibodies, but their plasma membrane contains receptors, which bind antibodies produced by plasma cells). If these antibodies come into contact with their antigens, they induce the release of the contents of the basophil granules. Eosinophil [granular type] 0%-5% of WBC The presence of antibody-antigen complexes stimulates the immune system. Eosinophils phagocytose these complexes and this may prevent the immune system from "overreacting". Their granules also contain the enzymes histaminase and arylsufatase. These enzymes break down histamine and leukotrienes, which again may dampen the effects of their release by basophils or mast cells. MBP, which can also function as a cytotoxin, and its release by eosinophils may be involved in the response of the body against parasitic infections, which are accompanied by an increase in the number of eosinophils. Monocyte [non-granular type] 1%-9% of WBC Once monocytes enter the connective tissue they differentiate into macrophages. At sites of infection macrophages are the dominant cell type after the death of the invading neutrophils. They envelop and destroy micro-organisms, tissue debris and the dead neutrophils. Monocytes also give rise to osteoclasts, which are able to dissolve bone. They are of importance in bone remodelling. Platelets These assist in the arrest of bleeding. Thrombocytes, which adhere to the walls of damaged blood vessels, can release serotonin, a potent blood vessel constrictor, sufficient to close even small arteries. If platelets come into contact with collagenous fibres in the walls of the vessel (which are not usually exposed to the blood stream), they swell, become "sticky" and activate other platelets to undergo the same transformation. This cascade of events results in the formation of a platelet plug (or thrombus). Finally, activating substances are released from the damaged vessel walls and from the platelets. These substances mediate the conversion of the plasma protein prothrombin into thrombin. Thrombin catalyses the conversion of fibrinogen into fibrin, which forms a fibrous net. Platelets captured in the fibrin net contract, leading to clot retraction, which further assists in prevention of blood loss. Blood coagulation is a fairly complex process, which involves a large number of other proteins and messenger substances. Deficiencies in any one of them, either inherited or acquired, will lead to an impairment of blood clotting. The prothrombin time, which is also called protime or PT, is a test that is used to assess blood clotting. Blood clotting factors are proteins made by the liver. When the liver is significantly injured, these proteins are not normally produced. The prothrombin time is also a useful test of liver function, since there is a good correlation between abnormalities in coagulation measured by the prothrombin time and the degree of liver dysfunction. Prothrombin time is usually expressed in seconds and compared to a normal control patient's blood. Return to TOP |
|
Other specific and specialized tests may be used to make a precise diagnosis of the cause of liver disease. Elevations in serum iron, the percent of iron saturated in blood, or the iron storage protein ferritin may indicate the presence of haemochromatosis, a liver disease associated with excess iron storage. In another disease involving abnormal metabolism of metals, Wilson's disease, there is an accumulation of copper in the liver, a deficiency of serum ceruloplasmin and excessive excretion of copper into the urine. Low levels of serum alpha1-antitrypsin may indicate the presence of lung and/or liver disease in children or adults with alpha1-antitrypsin deficiency. A positive antimitochondrial antibody indicates the underlying condition of primary biliary cirrhosis. Striking elevations of serum globulin, another protein in blood, and the presence of antinuclear antibodies or antismooth muscle antibodies are clues to the diagnosis of autoimmune hepatitis. Finally, there are specific blood tests that allow the precise diagnosis of hepatitis A, hepatitis B, hepatitis C, and hepatitis D. Return to TOP |
Last updated 11/06/2010
This page contributed by Liver Recipient #27.